Sunday Blog 133
Ruminations on informed consent
You can listen to this on the link below
“What’s been your involvement with pelvic mesh?” I was asked this week. A conversation among women gathered to walk the local labyrinth on the night of the (Pink) full moon, the subject had turned to someone who “had” to get surgery for pelvic organ prolapse.
I’ve never forgotten the moment in 2016 when I first heard about the pelvic mesh scandal. As an advocate, I knew this was going to be big.
In 2017, a Senate Inquiry into pelvic mesh was established, instigated by the courage and passion of several mesh-injured women. Part of the Inquiry was to find out how many mesh-injured women there were. We still don’t know. We may never know.
I had a role supporting women to put in submissions to the Inquiry, then attended the Inquiry to listen to those of them that had a slot to speak. I watched women sitting, then standing, shifting to find a comfortable stance, grimacing from the pain. By then I knew they’d have to rest for several days or a week after the exertion of attending the Inquiry in person. I’ve never forgotten the sobs of women, triggered through having to go through their stories again.
Then I too, gave evidence as a systemic advocate. As I sat in front of the panel, I could feel the women who all sat behind me. What a pressure and privilege it was, being able to speak for ten minutes as a systemic advocate. I wanted to do justice to their stories.
And then, the Senate Inquiry Report eventually emerged out the other end. I joined committees established to implement recommendations. Tried to help set up a woman-friendly mesh clinic in WA, with the miniscule funds set aside for the purpose. Over time, I noticed recommendations were actioned enough to pass administratively for “done”, while nothing much changed for women. (Check these links if you want to find out more on the Australian Commission on Safety and Quality in Health Care and TGA websites).
I watched on as the Shine Class Action emerged, and through the subpoena process, Shine could get medical records from all the states and territories, with enough cases identified to proceed. Apparently, we can’t use this data for the public good, to determine once for all the number of mesh-injured women. It can only be used by legal firms for the class action. Shine emerged with an enormous chunk of the settlement due to go back to them as fees. It was seen as so rapacious that they have now been stripped of the role of administrating the settlement to women. But the amount that women are now looking at receiving, minus the Medicare payments which they will have to return, is, frankly, an insult.
I’m involved with the Australasian Pelvic Floor Procedure Registry, a Senate Inquiry recommendation to track women’s outcomes into the future. Because yes, mesh is still being implanted in women. This Registry, like most of Australia’s, isn’t mandatory, so numbers are only very slowly building. Once again, we may not understand how many women have had mesh implants and are doing well or not so well.
After watching the Four Corners episode on back pain and spinal procedures, I looked up the Spinal Surgery Registry. It is also not mandatory. It has 20 participating hospitals and surgeons and just over 4,500 patients recorded. But that’s since 2018 and will be just the tiniest tip of the iceberg of surgeries done in that time.
Being part of the pelvic mesh advocacy work taught me so many things. How many holes there are in our regulatory systems, where medications require a higher burden of proof to be approved by the TGA than do medical devices. How there is often no continuity for women who choose a surgeon to undertake the procedure but may struggle to get follow up care. When you’re not happy with the outcome, you may never want to see that surgeon again. He or she will be blissfully ignorant that there are any concerns. Mostly, these surgical outcomes or “patient journeys” will be invisible at a system level. Harm can go on with no one noticing. We just don’t have the data.
All of this fires my obsession with what we can do as individuals—give informed consent.
And that is what I have led today’s Sunday Blog with. Maybe someone will see this on socials and it might be the just-in-time advice they need.
Sunday Blog 133 - Pro-social, not anti-science
In readiness for the forthcoming Health Consumers’ Council Book Club event with Susannah Fox, I’ve been reading her book Rebel Health, a Field Guide to Patient-led Revolution in Medical Care. My biggest take away so far is the importance of this distinction as a patient advocate - I am not anti-science—I am pro-social. What this means to me is that I believe in the vital importance of patients, family members & carers and lived experience advocates to be decision makers in all aspects of how our health system works. I believe the way we care for each other in our communities helps us to stay healthy. I also believe that there are many incredible treatments and passionate, caring clinicians who are keen to help us with our health issues. We need to work in partnership where we can, but rebel when the door is locked against us.
A recent spate of Four Corners episodes on health has been confronting. Apparently fraudulent or at least incompetent billing practices. Spinal surgery leaving people much worse off.
It all starts with us as patients giving informed consent. But how do we manage the yawning gap of medical knowledge between our surgeons and ourselves? How can we ask the right questions when we don’t know what we don’t know?
Do we understand what we are hoping to get out of the surgery, about what’s important to us? Are we eager to buy a “quick-fix” solution to our problem? Will we be able to stop and think? Will the expensive fifteen-minute appointment with our specialist, that perhaps we’ve waited months for, be enough time to fill in all the gaps?
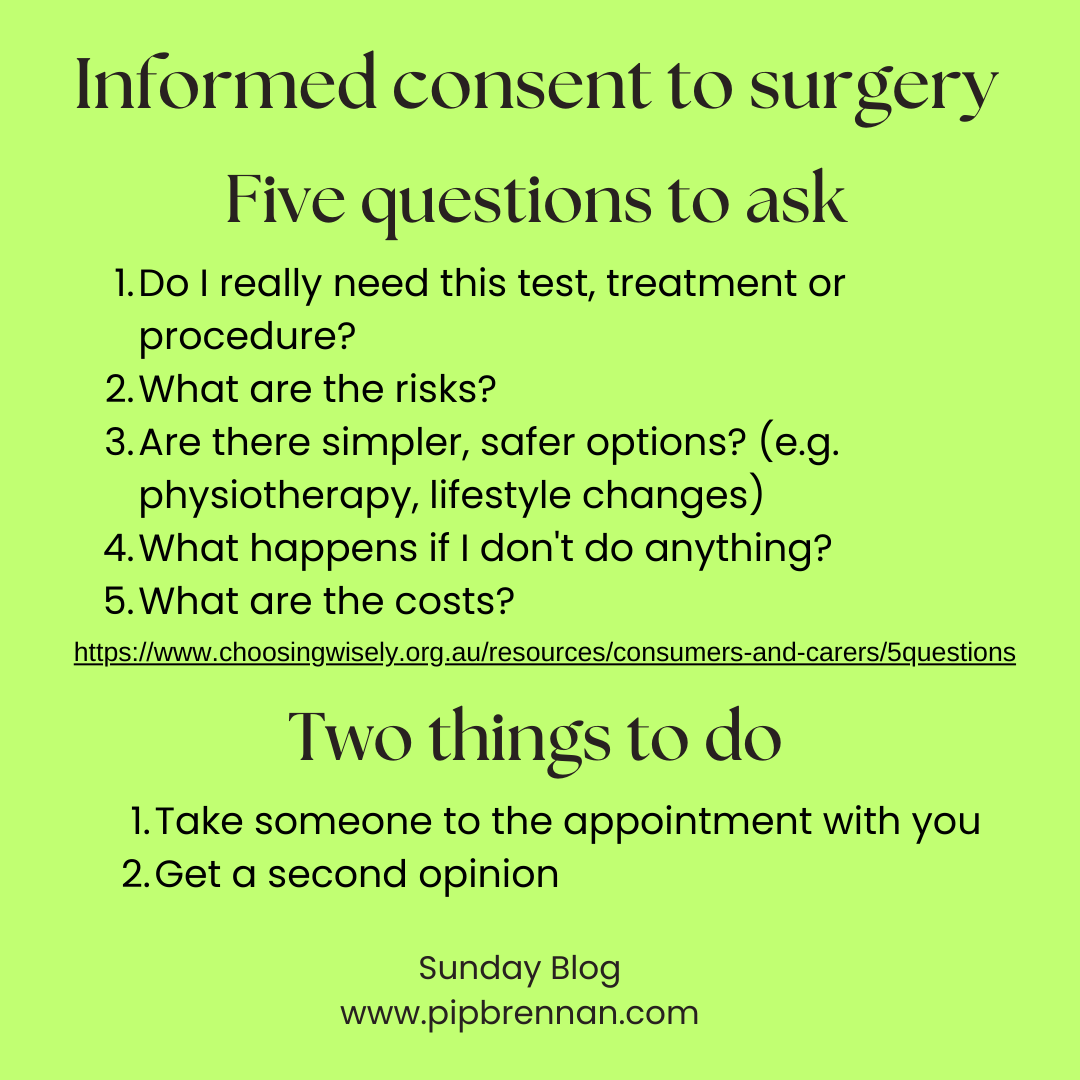
Everyone’s circumstances are unique, and there are no quick fixes to thinking through our options carefully. And yet five questions can be all that’s needed to guide us towards the right solution.
Do I really need this test, treatment or procedure?
What are the risks?
Are there simpler, safer options? (e.g. physiotherapy, lifestyle changes)
What happens if I don't do anything?
What are the costs?
I would add to this:
Take someone along to the appointment so they can take notes or record conversation on the phone to reflect on afterwards.
Get a second opinion—this may not please your surgeon. Don’t worry about that. You have to live with the consequences for the rest of your life. They may never see you again after the surgery is done. (I did a whole blog on second opinions you may want to dip into)
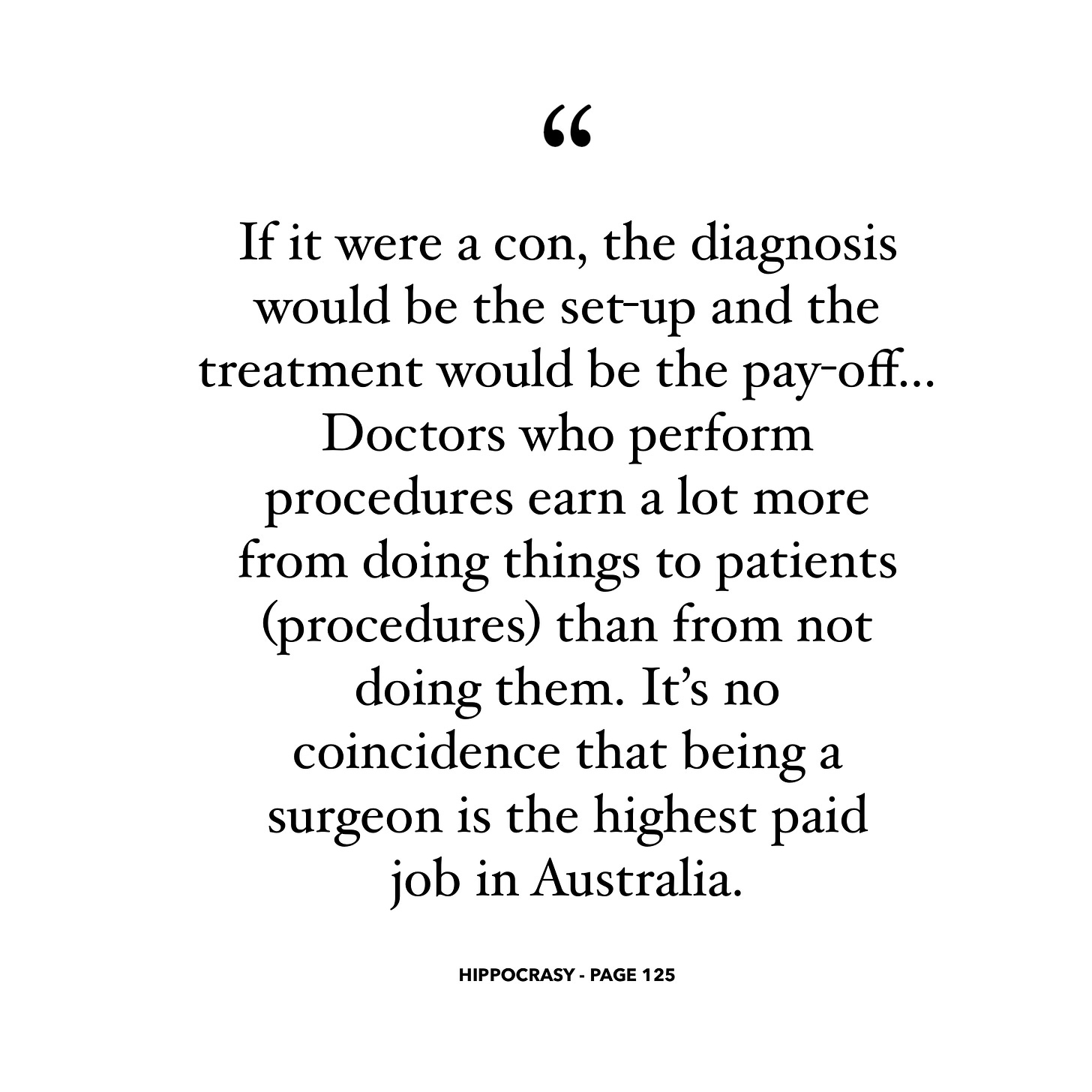
The last word belongs to the two doctors who wrote Hippocrasy—How Doctors Are Betraying Their Oath. One author, Ian Harris, appeared on the spinal surgery Four Corners episode.